Burning Mouth Syndrome – Trigeminal Neuralgia
The following sections aim to address any questions or concerns you may have regarding our highly effective non-surgical therapy treatment protocol for Burning Mouth Syndrome – Trigeminal Neuralgia. To fully understand the complexities of Burning Mouth Syndrome – Trigeminal Neuralgia, its effect on nerves and muscular fascia, its origin and its causes, we encourage you to explore each section.
(Tap or click to scroll to section)
Section 1: Burning Mouth Syndrome – Trigeminal Neuralgia Therapy Treatment Protocol
Section 2: Understanding The Complexities of Burning Mouth Syndrome
Section 3: Understanding Fascia
Section 4: Myofascial Adhesions: Source of the Problem
Section 5: Causes of Burning Mouth Syndrome
Section 6: Our Treatment Technologies
Section 7: Your Next Step
Section 8: Testimonials
Section 1: Burning Mouth Syndrome – Trigeminal Neuralgia Therapy Treatment Protocol
We remedy Burning Mouth Syndrome – Trigeminal Neuralgia by applying Shockwave Therapy treatments to disintegrate adhesions in the neck and jaw. Our therapy treatment protocol for Burning Mouth Syndrome (BMS) is a highly succesful protocol, refined over the past 15 years studying and treating this complex condition.
Burning Mouth Syndrome is a debilitating condition where the trigeminal and/or facial nerves are damaged due to various causes. Resolving it requires a dynamic diagnostic process and treatment protocol.
The most common causes we have identified for BMS over the years were due to neck arthritis, whiplash and its long-term affects, and chronic stress. (Section 5: Causes of Burning Mouth Syndrome)
Our dynamic treatment protocol addresses soft tissue damage in the neck and jaw, structural faults involving vertebrae/discs/jaw, and most importantly, damaged nerves. (see more below – 4. Addressing Root Causes)
________________________________________
Our Therapy Treatments Will:
1. Break Apart Adhesions responsible for nerve compression, if present.
2. Remove Damage (inflammation/scarring/trauma/sclerosis) from nerves, preparing them for regeneration.
3. Regenerate the Nerves to restore normal function.
4. Address Primary Root Causes contributing to BMS.
________________________________________
1. Breaking the Adhesions
We apply shockwave therapy, a technology originally developed to break apart kidney stones, to disintegrate adhesions in the neck and jaw. The applicator we exclusively use for shockwave therapy treatments is manufactured by EMS Technology in Germany. Considered the worldwide authority on EMS technology, they hold the original patents developed over 40 years ago.
Shockwave therapy treatments target collagen bonds within adhered fascial fibers, which can compress the trigeminal and facial nerves as they pass through the neck to the jaw and face. (Section 4: Myofascial Adhesions: Source of the Problem)
Treatment Process:
A gel is applied to the skin over the adhesions , then an hand-held applicator is depressed against the skin to begin producing the acoustic waves required to reach deep into the hardened adhesions.
Sessions begin with low-intensity waves, gradually increasing in intensity and depth to effectively treat all muscular adhesions in the neck and jaw area.
Having administered over 300 million shockwaves to date, Glenn uses the highly sensitive touch he developed learning braile and shockwave application skills, to monitor your responses and adjust the treatment parameters accordingly to ensure optimal outcomes.
Treatments ensure the return of normal blood flow to the neck and jaw, allowing essential oxygen for both muscle and nerve regeneration, as well as for the outflow of metabolic waste products.
________________________________________
What to Expect During Therapy Treatments
Throughout treatment, you may feel slight pressure as adhesions are broken apart, with immediate relief from symptoms. Our founder uses advanced palpation skills to locate and monitor adhesion dissolution and to adjust treatment as needed.
You will experience re-creation of your specific symptoms (burning/pins & needles/taste of metal) as we break apart adhesions responsible for those symptoms. Then within minutes you feel the enormous relief to your mouth as the nerve no longer causes those sensations. It is an amazing experience.
________________________________________
Post-Treatment Effects
You can expect skin tenderness, and perhaps slight swelling in the regions of the adhesions for up to 4 days following the first treatment. This is an essential part of the treatment process as we want the body to respond by swelling so the broken collagen proteins can be removed from the treated region by the lymphatic system, and the tissue regeneration phase may then begin.
Every subsequent treatment thereafter will trigger far less symptoms. This is because only adhered tissue cause the symptoms (reaction), healthy tissue causes none.
Treatments are designed to fit seamlessly into your daily routine, with no need to alter your activities. The effectiveness of our EMS shockwave technology provides significant symptom relief, often immediately after treatment.
________________________________________
2. Preparing the Nerves for Regeneration
Specialized electrical frequency technology is used to prepare the trigeminal and facial nerves for regeneration by:
• Removing chronic inflammation and calcification from the nerve body
• Removing fibrosis/sclerosis from nerve cells
• Restoring normal blood flow and oxygen to encourage healing
• Normalizing ion flow to return nerve function
This phase involves placing wet towels on the neck and stomach to allow electrical impulses to penetrate the body. The microcurrent is painless and imperceptible.
________________________________________
3. Regenerating the Trigeminal and Facial Nerves
Using world-leading nerve regeneration technology, we stimulate nerve repair and restore normal function. Sticky pads placed on the neck near the nerve exits deliver gentle electrical impulses, creating a slight buzzing sensation as regeneration begins.
________________________________________
4. Addressing Root Causes
BMS often arises as a secondary condition resulting from primary issues. Common root causes we’ve identified include:
• Chronic neck/jaw adhesions from long-term stress
• Neck arthritis
• Complications from whiplash
• Dental implants or extractions
• Chronic shoulder problems
In this final stage, we treat each individual’s specific causes as determined by our assessment. Using a combination of our technologies, we tailor treatment to achieve the best outcomes.
For a more detailed, case-specific explanation, we will provide a personal assessment and treatment plan after your initial evaluation.
Section 2: Understanding The Complexities of Burning Mouth Syndrome
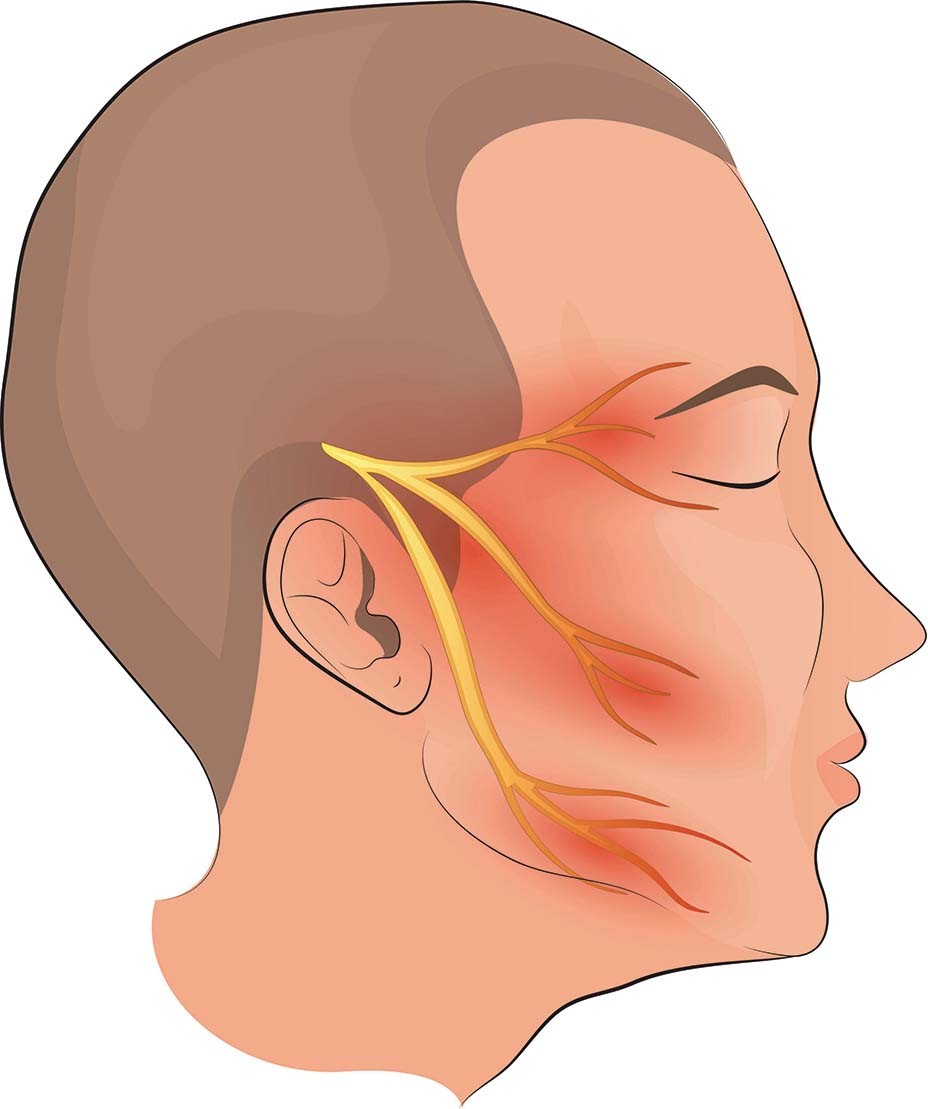
To begin, it’s important to note that two distinct nerves provide all sensory functions to the mouth and entire surrounding region. These two nerves are the trigeminal and facial nerves.
Trigeminal and Facial Nerve Anatomy
The trigeminal nerve and its branches provide sensory functions to the skin of the lower face and jaw, teeth and gums, tongue, salivary glands, palate, mandible (jaw bone), and skin of the chin and lips. The facial nerve provides sensory functions to the skin on the upper face, nose, eyelids, and surprisingly, a portion of the tongue as well.
Both nerves exit the brain through openings at the base of the skull and travel through the muscles of the upper neck, around the ear, and deep into the jaw before entering the jaw and face.
All peripheral nerves are comprised of both sensory and motor fibers. Motor fibers carry neurological impulses to cause muscles to contract, while sensory fibers carry impulses for every sensation we feel. Burning mouth syndrome is a nerve compression condition affecting the sensory fibers of both the trigeminal and facial nerves.
When nerves are physically compressed, stretched, or chemically irritated by agents such as chemotherapy, high sodium/glucose (diabetes), or decreased oxygen levels, they produce specific symptoms depending on the affected nerve fibers.
For example, nerve fibers that carry hot/cold sensations to the brain are responsible for the burning sensations experienced anywhere in the body, including the mouth (burning mouth syndrome). Other nerve fibers that carry taste sensations are involved when burning mouth sufferers taste metal or other unusual tastes, including blood. Dry mouth occurs when the nerve fibers controlling the salivary glands are affected.
Here is a comprehensive list of sensory functions that the trigeminal and facial nerve fibers are capable of sensing:
- Temperature: Hot/cold – Burning
- Pain: Dull Ache/Throbbing to jawbone, teeth, tongue, face…
- Itch/tickle
- Pins/Needles/Total Numbness (like dental anesthesia for cavity work)
- Taste: Metals, blood, salt, bitter, sweet, and other odd combinations, or a complete loss of taste
- Light Pressure
- Deep Pressure: Deep jaw/teeth ache
- Sharp Shooting Electrical Sensations
- Dry Mouth: (Salivary)
- Proprioception: Sensing jaw dislocation, inability to fully open the jaw…
- Bugs Crawling Sensations
- Dry Skin on Face and Jaw

As you can see, the symptoms of burning mouth syndrome are the result of facial and/or trigeminal nerve dysfunction. The muscles and their protective fascia in the entire neck region develop problems that directly affect the pathway of the nerves as they pass through this tissue from the base of the neck and clavicle up to the face and jaw.
The key to understanding burning mouth syndrome and its causes is understanding muscle health and the fascia that every muscle is comprised of.
Section 3: Understanding Muscular Fascia
Fascia is an extremely robust yet pliable type of connective tissue, predominantly comprised of collagen and elastin fibers. It intricately envelops and safeguards every living muscle and nerve fiber (cell) within the body’s muscular framework.
While collagen provides the necessary strength to shield and protect these sensitive muscle and nerve cells, elastin allows for the essential stretching and contracting ability that every muscle and nerve requires.
The prefix “Myo” pertains to the fascia associated with muscles, derived from the Greek term for muscle. Remarkably, a single muscle may contain upwards of 500,000 living muscle cells, each encased within a protective fascial covering known as endomysium. Clusters of these fascia-wrapped muscle cells, numbering around 20,000 in each bundle, are encased by another layer of fascia called epimysium. Finally, the entire muscle ensemble is enveloped by a third type of fascia called perimysium, which gives each muscle its distinct shape.
At all three levels, fascia serves to bind and protect the living muscle cells. Muscular fascia has excellent blood flow, facilitated by the vascular network of the living muscle cells, which supplies essential nutrients to the collagen and elastin fibers within the fascia. This system ensures that muscular fascia is adept at absorbing forces exerted during muscle contraction or stretching, allowing for the joint movement and work that muscles perform.
Section 4: Myofascial Adhesions – Source of the Problem
Myofascial adhesions, commonly known as adhesions, are regions of severely hardened and adhered fascial fibers amidst otherwise healthy, elastic fascial tissue. The ratio of collagen and elastin changes, resulting in more inflexible collagen fibers and fewer elastic, pliable elastin fibers. The result is a phenomenon where normally straight, healthy muscle fibers see an influx of new collagen fibers that twist and bind other fibers together like glue, forming an intricate weave of cross-bridged collagen fibers that changes the muscle’s tissue structure.
These adhered fascial fibers create dysfunctional, inelastic, fibrotic, and ischemic bands or large regions within the muscle’s fascial connective tissue layers and even throughout the entire muscle. The term adhesion (adhesive) commonly associated with glue aptly describes this phenomenon.
Adhesions typically form in the fascial tissue layers due to excessive and repetitive strain on its muscular fibers. The cross-bridged collagen fiber influx is the body’s unique method of protecting the living muscle cells from damage, as living muscle cells can die, leading to muscle wasting and atrophy.
The result of all this hardening, glueing, twisting, and deformation of a muscle causes:
- Entire muscle to shorten, severely crushing free nerve endings within the muscle, resulting in localized pain
- Decreased healthy oxygen flow into the muscle, causing pain
- Decreased outflow of metabolic waste, causing pain
- Entire muscle to shorten, crushing underlying nerves, arteries, and veins (Burning Mouth Syndrome)
Adhesions: Understanding the Consequences of Overstrain
Muscles are marvels of biomechanical engineering, capable of generating significant force to facilitate daily activities. However, this remarkable capacity comes with a caveat: muscles require time to recuperate from the stresses placed upon their fascial network, which protects the living muscle cells. Given adequate time, fascia can heal from the strains induced by vigorous activity. The issue lies in the time factor; frequently, we fail to allow our muscles and their fascia the necessary recovery period amidst daily demands.
Fortunately, the human body possesses an innate resilience, designed to safeguard every living muscle cell under duress. When myofascial tissue is deprived of sufficient recovery time, the body initiates a compensatory mechanism, generating new collagen fibers that intertwine individual fascial fibers in a cross-bridged pattern. This process fortifies the fascial network by binding individual muscle cells and their fascial coverings together, enhancing overall structural integrity.
These cross-bridged collagen fibers act as natural adhesives, binding groups of fascial fibers together to form a cohesive, robust unit, thus shielding the strained fibers from further damage. The term “adhesion (adhesive),” commonly associated with glue, aptly describes this phenomenon, where fascial fibers become bound together, reinforcing the tissue against overexertion.
Consequences of Adhesion Formation & Burning Mouth Syndrome
The formation of adhesions initiates a cascade of consequences, as these fibrous connections begin to compress the arteries, veins, and free nerve endings within the layers of fascia surrounding muscles and the neurovascular bundle that lies beneath. Consequently, a persistent low-grade pain manifests whenever muscles affected by adhered fascia are engaged. Additionally, these adhesions have the propensity to shorten certain bands of fascial fibers, exacerbating discomfort upon contraction or stretching of the affected muscles.
With Burning Mouth Syndrome, the repetitive strain adhesion formation can be attributed to various activities, including:
- Prolonged periods of computer usage with poor ergonomics
- Sustained tilting of the head to view a phone screen
- Engaging in sports without proper muscular conditioning
- Strain imposed by poor posture
- Emotional stress
- Breast enlargement
- Post-breast cancer surgery
- Substantial weight gain
- Chemotherapy
- Dental procedures
Each of these activities contributes to the overstrain of the muscles in the neck, jaw, and face, which have very thin layers of fascia. Over time, the fascia hardens and shortens, entrapping the delicate nerve fibers of the trigeminal and facial nerves.
The sensory dysfunction of these nerves leads to various symptoms such as burning, dull pain, pins and needles, dry mouth, metallic taste, and others associated with burning mouth syndrome.
Section 5: Causes of Trigeminal Neuralgia – Burning Mouth Syndrome
As stated above, the most likely cause of burning mouth syndrome is due to nerve entrapment, compression, and ischemic deprivation of the trigeminal and facial nerves as they travel through the fascia and muscles of the neck, jaw, and face.
The most common cause of repetitive strain injury and adhesions of the fascia and muscles of the face, jaw, and neck is sustained poor posture. With poor posture, the muscles of the neck and upper back remain in a semi-contracting state, causing them to stiffen and shorten. This leads to the overstrain of the fascia, which eventually leads to the formation of adhesions.
While posture may be the most common cause, there are other contributing factors to developing myofascial adhesions in the muscles and fascia of the face, jaw, and neck that lead to burning mouth syndrome.
These factors include but are not limited to:
- Emotional Stress
- Breast Enlargement
- Post-Breast Cancer Surgery
- Substantial Weight Gain
- Chemotherapy
- Dental Procedures
- Long Computer Sessions
- Neck Arthritis
Additionally, neck trauma, such as whiplash or falls, can lead to an almost immediate onset of symptoms due to the injury’s impact on the fascia, muscles, and nerves in the neck, jaw, and face.
Section 6: Our Treatment Technologies
How does the technology used to treat my condition, affect my chances of a cure?
What is the Innovative Therapy Canada difference?
Our Technologies
The two most important factors to your recovery are accurately and competently identifying root causes for your chronic pain, and then treating them using the most effective technologies the world has to offer.
So aside from a competent diagnosis, the technologies and how they are used are the most important part to the process.
EMS Swiss Dolorclast Extracorporeal Shockwave Therapy (ESWT)
Extracorporeal shockwave therapy, initially developed in the 1980s to fragment kidney stones (lithotripsy), is the therapeutic use of unique high energy acoustic (sound) waves to break apart extremely painful myofascial adhesions and unwanted calcifications in the soft tissues and joints of the body.
We use EMS Swiss Dolorclast shockwave Therapy, originators of the technology in Germany over 40 years ago, Because it produces the most effective and deep penetrating impulses among all acoustic shockwave generators worldwide. EMS technology is patent protected, so no other shockwave therapy devices are allowed to copy the brilliant engineering that EMS originally engineered.
The acoustic waves are created by propelling a metal projectile with high pressure compressed air (up to 120 PSI) through an exceptionally long cylinder within the applicator to strike an alloy tip. These acoustic impulses are transmitted to the body through a conductive gel applied to the skin over the region to be treated.
Its powerful acoustic waves create a distinctively high-pressure wavefront, triggering rapid expansion of blood/lymphatic gas molecules in fibrotic adhered tissue, followed by a rapid implosion force.
This rapid expansion/implosion wave cycle (shockwaves) results in the creation of beneficial fascial adhesion tissue disruption effectively degrading the collagen bonds of adhered fibres, causing them to disintegrate.These myofascial adhesions along with tendinopathies, heel spurs, pinched nerves, general muscle fibre damage, ligament sprains, chronic inflammation, and pinched nerves are all examples of how widespread chronic pain can manifest itself in knees, hips, low back, neck, arms, and legs. Shockwave therapy is the only technology able to break apart the core dysfunctions responsible for most chronic pain conditions.
Physiologically, the healthy tissues of nerves, smooth muscle and outer fascial connective tissue layers of organs, ligaments, tendons, blood vessels, and lymphatic channels possess varying degrees of elasticity and can expand without harm as shockwaves traverse their cellular structures. Shockwaves have no affect on bones.
We have enhanced the therapeutic use of this world class technology over the past 20 years, having administered over 250 millions shockwaves to every region of the body. We have engineered and offered safe and effective treatment protocols to break apart painful, debilitating myofascial adhesions crushing nerves, exerting damaging forces on joints, squeezing and restricting essential blood flow, and break apart unwanted and painful calcifications, anywhere in the body.
Its astonishing, unrivalled capability of our EMS technology, coupled with our founders unique ability to feel dysfunctions, is one of the most important reasons why we at Innovative Therapy Canada solve the chronic pain conditions we do.
Trigenics Myo-Neural Therapy
Trigenics is an advanced neuromuscular (nerve & muscle) therapy, implemented to restore normal neurological communication between brain and muscles during the soft tissue regeneration phase of our treatment protocols.
It involves the physical application of pressure supplied by a unique, cam-gear driven thruster technology administered to regenerating muscles and tendons.
Highly specialized neurological receptor cells embedded within muscles, tendons, and ligaments repaired in our treatment protocols need to be re-set to return normal function.
Trigenics corrects muscle imbalances restoring skeletal equilibrium essential to any body recovering from chronic pain.
Spinemed Professional Computer-Guided Spinal Decompression system
This highly specialized technology from Spinemed is the world’s most effective computer-guided spinal decompression technology. It encourages bulging/ruptures spinal discs to heal from a variety of potential causes.
Spinal discs are prone to degeneration and injury over the years as they are constantly compressed and twisted through daily activities.
As a disc degenerates, the fibrous water-filled interior loses some of its water, bulging like a car tire that has lost air. It also reduces disc height creating instability to that section in the spine thus causing ligament strain and pain.
Disc degeneration also causes the elastic outer disc lining to become brittle and susceptible to cracks and tears that can lead to disc herniations.
Bulging or herniated discs can then press on exiting spinal nerves, causing severe pain.
Damaged intervertebral discs will not heal if the abnormal forces being exerted on them is not identified and removed.
Our therapy treatment protocols are designed to identify these unwanted forces, remove them, then use the Spinemed decompression system to restore health to the involved discs.
Frequency Specific Microcurrent FSM
Frequency Specific Microcurrent is a very unique type of low-grade electrical currents therapy that encourages the repair of body tissues at a cellular level.
It is not TENS, not ultrasound, not shockwave, not laser, and not stimpod. It is a technology all on its own, developed in the 1920’s.
FSM uses bursts of electrical energy at very specific frequencies to encourage cellular changes breaking down cellular obstacles that interfere with the regeneration process. This then helps the body heal.
The electrical energy propagates through the body by resonating in the 88% water content we are comprised of, like when a rock is thrown into a pond.
This energy is in the form of exact frequencies which target specific cells that respond to these frequencies. For example, nerves respond to a frequency of 396 cycles per second.
Each type of cell responds to a specific frequency which is how the technology can affect specific body parts to help them heal.
FSM is yet another essential tool we have in our chronic pain therapy tool box that we use extensively to solve issues from the brain to the feet.
We rely on it to solve such conditions as traumatic brain issues caused by concussions, whiplash, neck/skull fractures, and neck arthritis.
Rebuilder Medical Nerve Regeneration
The nerve rebuilder is another highly specialized electrical therapy technology we used extensively to resolve peripheral nerve neuropathy, and to encourage the regeneration of severely damaged peripheral nerves, common to most who suffer from chronic pain.
We use this unique technology in the final stages of our treatment process to encourage regeneration of peripheral nerves by:
- Wakes up dormant nerve cells and restore normal polarity along the nerve axons and dendrites. This helps nerves transmit signals properly again.
- Relaxes and re-energizes shrunken nerve cells by increasing blood flow and oxygen to the synaptic junctions between nerves. This provides nutrients for nerve repair.
- Stimulates muscles (along with nerves) using specific electrical signals. This causes the muscles to contract and relax which results in an increase in blood circulation.
Section 7: Your Next Step
Your journey towards relief begins with taking the next step. Here’s what you can do to initiate the process:
Contact Us:
Reach out to us to schedule a consultation and initial treatment session. Whether you’re local or from afar, we’re here to assist you in finding the best solution for your condition.
We encourage calling us from a land-line phone or e-mail. Cell phones go through dead zones and often our voice message system fails to hear the entire message including a return phone number.
Consultation and Treatment Plan:
During your consultation, we’ll discuss your specific situation in detail and work together to formulate a personalized treatment plan tailored to your needs.
Since treatments require intervals between sessions, we’ll address the logistics to ensure seamless administration of treatments.
Flexible Treatment Options:
Treatments can be administered at any time, even during flare-up situations. Our initial treatment is designed to swiftly reduce painful causes, providing immediate relief.
There’s no “bad” time to begin treatments. The sooner you start, the sooner you’ll experience resolution and regain control over your life.
For more information on our treatment for this condition, or on any other chronic pain condition you may suffer from, we encourage you to contact us to discuss options available to you.
By the time she came to see us, she was at the end of her rope. I recall her telling me in her soft voice that I was her last hope.
(click to here view Ann’s full story)

